04 Feb Preventing the Spread of Infections Through Proper Sharps Handling
Although not part of Standard Precautions, it seems appropriate to discuss sharps handling after discussing safe injection practices in an earlier blog. While safe injection practices focus on protecting patients from poor healthcare personnel practices, this blog focuses on protecting the healthcare worker.
Some Basic Information on Sharps
The Occupational Safety and Health Administration (OSHA) Bloodborne Pathogen Standard became federal law in 1991. The 2001 update, which was published as the Needlestick Safety and Prevention Act, primarily clarified portions of the original standard. However, even with such an emphasis on prevention, sharps injuries among healthcare workers are still common. The Centers for Disease Control and Prevention (CDC) estimates 385,000 sharps injuries occur every year in U.S. hospitals. When considering all healthcare settings, healthcare workers experience 600,000 to 8000,000 sharps injuries annually in the United States.
Which occupational group most likely to experience a sharps injury, really depends on the sharp. The most recent sharps and needlestick injury data indicates that sharps injuries occur more frequently among nurses (35%), interns/residents/fellows (17%), attending/staff/specialty physicians (16%), and surgical attendants (9%) than other occupational groups. Additionally, about 25% of sharps injuries occur among non-users such as environmental service (EVS) technicians, waste haulers, and laundry personnel.
As expected, disposable syringes were involved in 24% of the reported injuries, and suture needles were involved 25% of the time. This seems to be in line with nurses and physicians experiencing the most injuries compared to other occupational groups. Another category, sharp instruments, caused injury 11% of the time.
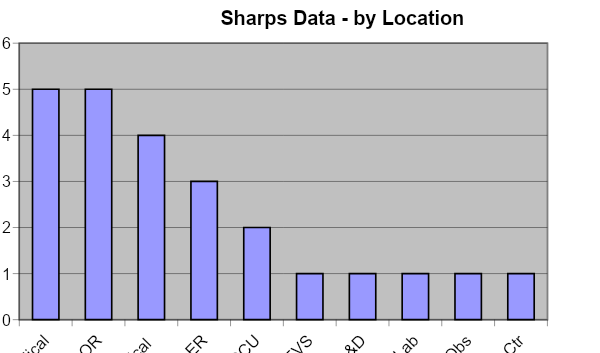
Injuries occur most frequently in the Operating Room/Recovery (44%), patient rooms (22%), Emergency Department (9%), outpatient clinics/offices (7%), and procedure rooms (6%). Other areas experienced sharps injuries in much smaller numbers.
Quick Facts About Sharps
Some other interesting facts about the information submitted to the International Healthcare Safety Center:
- Fifty-nine percent of the sharps involved in incidents were not a safe design with a shielded, recessed, retractable, or blunted needle or blade.
- For the sharps that had a safety design, 66% did not have the safety mechanism activated, and 23% were only partially activated. By contrast, only 9% had the safety mechanism fully activated at the time of injury.
- The majority (46%) of the injuries occurred before activation, while 33% occurred during activation.
At this point, you may be thinking that all these numbers are ‘nice to know,’ but what does that have to do with you and your facility! Let’s explore a little further.
Exploring Sharps in Your Facility
Most, if not all, facilities collect sharps injury data. Some facilities collect a lot of details, while others will collect very sparse information about each incident. According to OSHA, the sharps injury log must contain the type and brand of device involved in the incident, the department or work area where the exposure occurred, and an explanation of how the incident occurred. Although it is true that not all healthcare facilities must maintain an official OSHA log, the basic information shouldn’t really change since it is the same information that will help you to figure out how to decrease sharps injuries.
Many facilities find it helpful to group injuries by the occupational group as well as the above information. The real question becomes: What happens to the information once it is collected? The sharps information, regardless of whether an OSHA log must be maintained, should be collated and analyzed so it can be understood and used to decrease sharps injuries. The next logical question should be: “Are we collecting the correct information to make informed decisions for improvement?” Many times, facilities collect so little information about each injury that it doesn’t prove very helpful to decrease this type of injury. The above information should be collected at all facilities, even if healthcare personnel is sent to a remote site for evaluation after an incident.
Helpful Data Regarding Sharps Injury
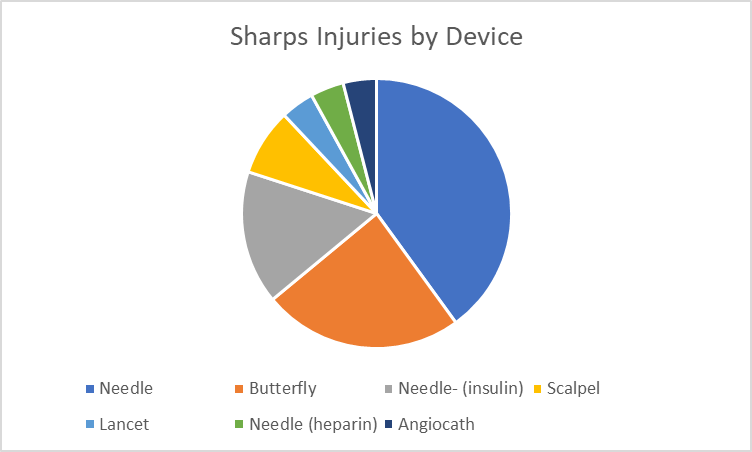
Some examples of how to collate and present the sharps injury data include the following:
Sometimes a simple table is very helpful:
| Sharps Injuries by Device | # of Injuries |
| Needle | 10 |
| Butterfly | 6 |
| Insulin needle | 4 |
| Scalpel | 2 |
| Heparin Needle | 1 |
| Angiocath | 1 |
Note: This is the same information that is presented in the pie chart above.
The important points are:
- Collect enough detail that the information or data makes sense to someone not directly involved in the sharps incidents
- Put the data together in a way that makes sense, depending on who will see the information.
What Can Be Done to Decrease Sharps Injuries?
Explore your data and look for commonalities. For example:
- Is a specific device the culprit in most injuries?
- Are injuries occurring despite the use of sharps safety devices? If so, does everyone know how to use the device and/or activate it properly? Talk to a sample of those using the safety devices to find out more information. Is there a better-designed safety device available?
- Are most injuries occurring in a specific area of the facility, such as the procedure room? If so, talk to everyone working in that area to help figure out the reasons.
If the area with the most injuries is an Operating Room, observe some surgeries to determine if a neutral zone or hands-free technique is used to pass sharps as recommended by the Association of periOperative Registered Nurses (AORN). This simply means that sharps are not passed directly from the Surgical Technician to the Surgeon or vice versa. Instead, the sharp is placed in a designated area such as a basin, instrument pad, magnetic mat, or specific area of the Mayo stand. This is where a sharp is placed rather than handed directly to the surgeon. Please note that implementing this type of change will take collaboration among all team members, time, and education.
A variety of assistance is available online if the data analysis reveals the need to find a new or better-designed safety device: evaluation forms for safer injections, sharps containers, and eye protection, the CDC offers a workbook for Designing, Implementing & Evaluating a Sharps Injury Prevention Program that assists with all aspects of a sharps injury prevention program and helps with OSHA bloodborne pathogen standard compliance.
Additionally, EPINet, which is part of the International Safety Center, offers report forms and free software for tracking and analyzing sharps injuries. Speaking of software, inpatient facilities can consider using the National Healthcare Safety Network (NHSN), offered for free by the CDC to track and analyze blood and body fluid exposures. NHSN can also track post-exposure prophylaxis information if your facility opts into that portion. Another good resource is the International Sharps Injury Prevention Society, which offers a safety product list as well as a list of additional resources.
Some Closing Thoughts on Sharps
Lastly, the OSHA Bloodborne Pathogen Standard mandates that frontline workers are involved in the identification, evaluation, and selection of engineering and work practice controls, and this must be documented annually in the Exposure Control Plan. Engineering controls are strategies or physical items that basically ‘force’ work to be done a certain way.
Work Practice controls govern how things are done, such as care in handling sharp devices. Using your data to guide improvements, talking to healthcare personnel, and documenting safety device evaluation results are all steps that will help move your facility toward compliance with the OSHA standard.
References:
- The National Healthcare Safety Network (NHSN) Manual. Healthcare Personnel Safety Component Protocol: Healthcare Personnel Exposure Module. Division of Healthcare Quality Promotion. https://www.cdc.gov/nhsn/pdfs/hps-manual/exposure/HPS_manual.pdf
- International Safety Center. 2018 Sharp object injury report. https://internationalsafetycenter.org/exposure-reports/
- AORN Guidelines for Perioperative Practice. Sharps Safety. 2019. https://www.aornguidelines.org/guidelines/content?sectionid=173724314&view=book
- AORN Frequently Asked Questions. Sharps Safety. https://www.aorn.org/guidelines/clinical-resources/clinical-faqs/sharps-safety (Can be accessed if not an AORN member).